When asked what I do for a living, I say I am a scientist and most people are intrigued and want to know more. When I then say I have worked at a brain bank for the last 10 years, I get a range of reactions. Some don’t know what that means (yes, literally a bank of human brains), some are fascinated and want to know exactly what a human brain is like and many just make a comment that it makes their job sound boring.
So, what is a brain bank? Brain banks are precious collections of human post-mortem brain tissue that have very kindly been donated when somebody has passed away. There is a whole network of brain banks in the UK and throughout the world. This network allows coordinated methodology and tissue requests across many brain banks, meaning more consistency with how brain tissue can be used within studies from multiple brain banks. By collecting the brain tissue, brain banks are able to provide a diagnosis to relatives and then use the brains in research projects to understand disorders that affect the brain and central nervous system.
Brain banks specialise in different aspects or different nervous system disorders. Within the UK for example are brain banks specialising in dementia, Parkinson’s disease, Multiple Sclerosis, Autism and Sudden death. As a dementia researcher, I work at Queen Square Brain Bank for Neurological Disorders [1]. We collect brains from a variety of parkinsonian disorders as well as a range of dementias.
During life, a patient will decide whether they want to donate their brain for research. They will provide informed consent and become a registered donor. At time of death one of the brain bank administrators will be in touch with the family and the mortuary to get next of kin consent and liaise to allow the donation to happen. Once a post-mortem has taken place, the brain is transported to the brain bank. From here one of our technicians will separate the brain into two halves so that the right half can be frozen and the left half can be preserved in a fixative. The reason for this is that different biochemical and molecular scientific techniques may need the tissue to be in a particular state, so by separating into halves, the most can be made from the valuable gift that somebody has given.
The frozen half will be cut into slices (5mm thick) from the front to the back of the brain and then frozen very rapidly on -80oC brass plates to stop any ice crystals from forming. This preserves the tissue for use for a long period of time. The other half will be placed in a fixative called formalin for three weeks so that the tissue is then preserved. This half of the brain will then be examined closely by a neuropathologist at a weekly brain cut session with assistance from a research technician. I performed this job when I was a research technician and learnt so much about the anatomy of the brain and the subtle differences that can be observed with the eye to decipher the different neurodegenerative diseases. This fixed half of the brain is also cut into 5mm slices, they are laid out and a preliminary diagnosis is given from examination by the neuropathologist. Most neurodegenerative diseases, and certainly many dementias, can only have a diagnosis confirmed at post-mortem due to large overlap between clinical symptoms and presentations between different types of dementia in life. This is why the first priority of the brain bank is to confirm diagnosis. This is then fed back to the family if they wish to know.
From the fixed slices, small blocks of tissue are collected from the main and important regions of the brain for further preservation such as areas affected in the diseases or areas of the brain that are important for brain function. These are then processed through a number of alcohols and chloroform to dehydrate the tissue and preserve it further before being embedded into paraffin wax. This process allows the tissue to be kept indefinitely. These wax blocks are then used to cut very thin sections of the brain tissue at 8 µm (1mm = 1000µm) that are loaded onto glass microscope slides. Proteins of interest are then stained using a technique called immunohistochemistry, utilising antibodies against the protein you are staining, to visualise these proteins underneath the microscope as shown in the image below.
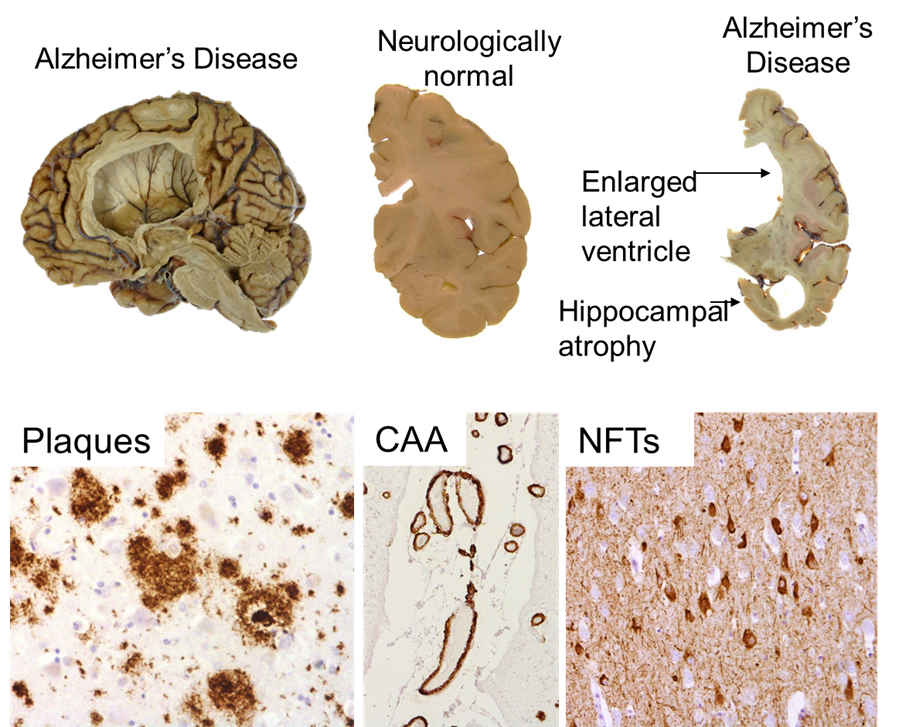
From top left to bottom right: Half hemisphere of an Alzheimer’s disease brain; 5mm slices from a normal brain and an Alzheimer’s brain; Immunohistochemistry of proteins found to accumulate in Alzheimer’s disease (amyloid beta – plaques in brain tissue and CAA in blood vessels, tau – NFTs in neurons)
In many neurodegenerative diseases, certain proteins accumulate into aggregates within the brain and this can be observed using a microscope. A neuropathologist will examine the slides that have been stained for proteins affected in the various diseases and use consensus staging criteria set out by multiple research groups to determine which disease the person had. This will be compared with the clinical notes for the patient and a final definitive diagnosis will be given. If the family have requested to know the diagnosis, our brain bank nurse will feed this back to them.
Once a diagnosis has been made, if consented for, the tissue can then be used for research purposes. Any researcher from the UK or worldwide can apply for the tissue via a tissue request but a committee has to agree that it is an ethical use of the brain tissue and that the study is robust and well designed. Once this has been agreed a material transfer agreement, a legal document will be agreed to make sure that all aspects of the Human Tissue Act will be followed. A team of administrators and technicians at the brain bank administrate this and process the tissue request before it is sent out to various research teams.
A great deal of research has been propelled forward by the use of post-mortem human brain tissue with many discoveries aiding better clinical diagnosis and understanding of disease processes being made. Needless to say, the gift of brain donation is not one that can be taken for granted and is the greatest gift to future generations that can be given. So, when somebody asks me about what job I do, that is the message I like to get across.
More information on the Queen Square Brain Bank [2]
Author

Dr Christina Toomey
Dr Christina Toomey [3] is a Post-doctoral Research Associate at University College London and The Francis Crick Institute. Having worked as a neuroscientist for 10.5 years, she is still as passionate as she started. Christina is an active member of the lab, in addition to teaching undergraduates, MSc and PhD students. She also works on widening participation and public engagement, through UCL and representing Alzheimer’s Research UK. Outside the Lab, Christina is a Brownie Leader, Netball Player and Science Tutor.