Hello there. My name is Ajantha Abey, I am a phd student at the University of Oxford, and it’s great to be joining the Dementia Researcher blogging team. For my first blog post, I thought I would share my 10 take aways from recent conferences. Over the last few months I’ve had the opportunity to go on something of a conference spree. They ranged from the local and affordable like the Oxford Neuroscience Symposium and DPUK’s Translation 23, online meetings like AAIC Neuroscience Next, and big international meetings like the ARUK Conference, ADPD 2023, and BNA International Festival 2023.
While there is the ever-present caveat of the impossibility of summing up all the exciting developments across the field, I have attempted here to put together my top 10 take-aways, both about the hot topics in dementia research, and about conferencing more broadly. It should be noted that I am certainly biased towards my own area of disease mechanisms, though I try to look beyond this and stay relatively broad and high-level, without going too much into depth into any one topic.
- Therapeutic Breakthroughs are Finally Happening
For many years now, the dementia and neurodegenerative disease field has been mired by the mirage of treatments that might emerge 5-10 years in the future. Finally, that vision is crystallising. From Lecanemab for Alzheimer’s Disease, or Tofersen for ALS, regulatory approvals and concrete clinical outcomes are at last coming through; while far from perfect, these developments are generating a huge amount of discussion, excitement, and energy. Far from the fatalism of five years ago when more and more companies were giving up on neuroscience, the recent breakthroughs have reinvigorated investment, brought renewed focus to the increasingly diverse pipeline of possibilities, and stimulated a lot of discussion (though not without controversy of course!).
- Some of the Most Exciting Advances are Happening in Fluid Biomarkers
As much as new therapies are significant, it would seem some of the most transformative work is happening in biomarkers. The recent advances in fluid biomarkers like phospho-tau in blood plasma for Alzheimer’s disease in particular could revolutionise testing, clinical trials, and timing of therapy. When standing next to disease mechanisms and drug discovery, the biomarker field is probably somewhat overlooked by the lay audience, but advances here are starting to enable earlier detection of disease, better definition of diverse patient cohorts in trials, and clearer stratification of trial participants. The proliferation of biomarkers relating not just to protein aggregation and neurodegeneration but also to inflammation is further giving us a more comprehensive understanding of disease [1] progression in human patients. All of these will enhance our ability to run better clinical trials [2] with therapies that have a better chance of working. It’s arguably the area enabling the biggest advances in the dementia research space at the moment.
- Digital Biomarkers Are on the Rise
An offshoot of the biomarker story that is still relatively niche but looking increasingly exciting is the space of digital biomarkers. While these haven’t gotten as much attention as their fluid counterparts, the increasing adoption and power of wearables (like smart watches) and personal digital technologies (like smart phones), alongside advances in simplifying complex hardware like electroencephalography (EEG) machines and the rise of cloud computing all seem to be enabling a lot of growth in this space. Digital and cloud-based neuroscience companies are attracting more funding, and while very early stage, exciting developments are occurring like prototype in-ear EEGs that could help overcome common issues such as compliance. Digital biomarkers have enormous potential to help remotely monitor patients, ease trial participation, and potentially eventually offer population level screening. One big issue this field has to face though is that of trust and privacy. As even more tools such as artificial intelligence and virtual reality technologies emerge for collecting and analysing individual data, it will be vital to consider how research and healthcare systems can best utilise mass data collection and maintain public trust in a world increasingly skeptical of ‘big’ tech, pharma, and government.
- Spatial Transcriptomics is the Hottest New Technique on the Block
In the land of disease mechanisms, ‘omics’ and big data is nothing new, but incorporating spatial data into single cell analyses is one increasingly popular development that is enhancing our ability to interrogate cellular level data. While genomics initially gave us genetic data [3] about individuals, then bulk RNAseq helped us understand broad changes in gene expression, and single cell approaches helped us identify which and how individual cells are changed in disease, the newest iteration in the ‘omes’ journey allows the interrogation of single cell gene expression in situ. This has opened up opportunities to examine cellular responses and interactions with nearby protein pathology and inflammation, explore questions around selective vulnerability, and visualize how diverse disease driving pathways relate spatially. It’s a very cool emerging technique and I’m excited to see more creative uses of it.
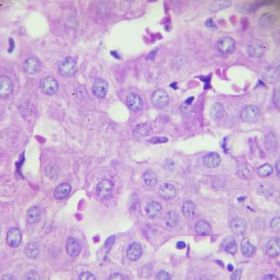
- Everyone’s New Favourite Cell Type is Microglia
First, it was the neuron, the logical focus of neurodegenerative disease research. Then came astrocytes, and a wave of interest in role of these helper cells in disease. Now, the time of the microglia has come. In Parkinson’s and especially Alzheimer’s, more and more genetic evidence points to an important role for these brain resident immune cells in disease [4] risk. The concurrent rise of induced pluripotent stem cell models for making patient microglia in a dish has aided this discovery boom, with cocultures of microglia with neurons and astrocytes, or organoid (“mini brain”) models incorporating microglia becoming noticeably popular. Alongside this is an increasing focus on the role of inflammation, the ‘inflammasome’, inflammatory biomarkers, and even suggestions that the Alzheimer’s ATN (amyloid, tau, neurodegeneration) definitional framework should be extended to ATNI, for inflammation. This has also gone hand in hand with the increasing interest in the role of the gut microbiome in recent years, especially for Parkinson’s disease and the role of inflammation there. In this light, it is incredible to watch one of the biggest shifts in the framing of these diseases – from proteinopathies to neuroinflammatory diseases – take place [5], and it will be fascinating to see research in the coming years on how the inflammation story intersects with the protein aggregation story to give us a more comprehensive understanding of these diseases. A popular line of investigation that seems to be bearing fruit is examining whether inflammation and glial dysfunction distinguishes between cognitively resilient and impaired individuals with similar levels of pathology.
- Lipids are an Emerging Frontier
A perhaps still relatively niche area that nevertheless appears to be attracting more attention and dedicated conference sessions is that of lipids. The last several years have seen a growing understanding that common risk genes in Alzheimer’s like ApoE, and Parkinson’s like GBA play a big role in lipid metabolism, and as such, efforts to understand lipid dysfunction in human, animal, and cell models is well underway. While still early days, this will surely be one of the key areas to watch in coming years, and points to the massive proliferation in our understanding of diverse disease mechanisms, from potential involvement of the gut microbiome and inflammation to the role of glial cells and vascular contributions to brain breakdown.
-
Recent developments in neuroimaging, fluid biomarkers, and ‘omics’ techniques have shed light on the heterogeneity of pathology in patient populations.
Pathological Heterogeneity & Conformational Strains are getting the Attention they Deserve
One of the themes developing from the last several points is that of disease heterogeneity, which has also featured as an explicit topic in recent conferences. Heterogeneity of pathology in patient populations is not new, but it is finally receiving the attention it deserves. This has been enabled by the emergence of neuroimaging and fluid biomarkers that are better able to distinguish patient subgroups, alongside developments in ‘-omics’ techniques and mass multiplex imaging allowing more in-depth assessment of copathologies in larger amounts of sample. Not only do we have a better appreciation for how the pathological milieu can differ between patients, but we can now better assess a diverse array of disease mechanisms associated with clinical outcomes.
A related area of attention seems to be in examining whether different conformational strains of aggregating proteins underly the diverse distributions of similar pathologies in different diseases (for example: alpha synuclein aggregates in Parkinson’s Disease vs Dementia with Lewy Bodies vs Multiple Systems Atrophy), also enabled by techniques emerging in recent years like correlated light electron microscopy, and various protein aggregation seeding assays. As our understanding of these diseases becomes more complex and more nuanced, working out how to integrate and interrelate different pathways and having people who can straddle different parts of the field will be increasingly important.
- We (still) rely a lot on genetic and rodent models
Despite our understanding of the myriad array of disease mechanisms expanding and an increasingly diverse therapeutic [6] pipeline, one thing that has not changed much is our reliance on genetic and especially rodent models of disease. It’s remarkable just how much data – across posters, talks, and trials – ends with the qualification ‘in mice/rats’. Even in human cellular models, we remain largely constrained to rare genetic disease variants, and in Alzheimer’s research, many tau models use truncated or mutant P301L tau (or similar), which do not reflect the conformational or genetic makeup of tau in the disease. On the one hand, a lot of this is done out of necessity, practicality, or utility. On the other hand, our increasing understanding of the complexity of mechanisms and pathology largely remains uncaptured by these models, and their translational record remains fraught. New ideas exist, including natural mammalian models, attempts to use live human brain slices from surgeries, and incorporating multiple different cell types in increasingly complex human cell models. Nevertheless, these remain rare examples and rarely discussed. Entire sessions devoted to new and emerging therapeutic strategies are exciting, but having all the data in these sessions based on the same genetic rodent models reminds us of the uncertain ground on which we stand. It would be great to see more attention in conferences paid to improving existing models and developing new ones that match our growing understanding of disease complexity and capture the diverse mechanisms that appear to be important for translational validity.
- Good moderators vastly improve a conference
Moderators are often an overlooked role in a conference session, but at ADPD 2023 in particular, moderators were fantastic and made me appreciate what an underrated effect they have on a conference. In the first instance, a good moderator can set the tone for an entire session, bringing energy and enthusiasm to engage the audience and contextualise a talk, especially vital in those after-lunch sessions, whereas a half-hearted moderator will only switch people off. Throwing in a few jokes, good or bad, can lighten the mood, create a collegial atmosphere, and help offset the need for moderators to be strict in their other vital role: controlling the timing of talks. Keeping speakers (especially the big-name ones) to time can be a daunting task, especially with interesting data or lots of questions and discussion to cut off, but keeping to the conference schedule is fairer on the speakers, makes it easier to swap between parallel sessions, and makes the entire experience smoother for everyone. The oft overlooked moderator thus holds a lot of power in conferences, and when used well, it can make all the difference.
- Inclusion is taking centre stage
Just as important as the scientific and research content is discussion about how we go about doing science and research culture itself. In this light, it’s great to see more conferences proactively headlining issues around diversity and inclusion in big plenary sessions, as well as paying attention to scientific practices like open data, reproducibility, and statistical approaches. In the massive field of dementia research, it is vital that these issues don’t get lost under all the exciting biology, because it is this very infrastructure of the research environment that produces that biological discovery – with better or worse outcomes. Despite some particularly egregious examples, it’s great to see that the ‘manel’ (panels made up entirely of men) is becoming a thing of the past, conferences are increasingly being designed to accommodate diverse [7] accessibility needs, and discussions on these issues are being put front and centre.

Ajantha Abey
Author
Ajantha Abey [8]is a PhD student in the Kavli Institute at University of Oxford. He is interested in the cellular mechanisms of Alzheimer’s, Parkinson’s, and other diseases of the ageing brain. Previously, having previoulsy explored neuropathology in dogs with dementia and potential stem cell replacement therapies. He now uses induced pluripotent stem cell derived neurons to try and model selective neuronal vulnerability: the phenomenon where some cells die but others remain resilient to neurodegenerative diseases.