Dementia is a term used to describe impairments in cognition which can be diagnosed using specially designed clinical tests and observations. What is more difficult to diagnose is the cause of the dementia; specifically, what is the brain disease which has led to the development of the dementia syndrome. Often a definitive diagnosis can only be confirmed post-mortem when the brain can be examined, but this is a problem if we want to provide specific and targeted treatment for people living with dementia. In this blog I will describe what neuropathology can tell us about the brain diseases which lead to dementia, and what this means for dementia diagnosis in life.
Dementia is an “umbrella” term for clinical symptoms relating to a specific impairment in memory function and other cognitive domains such as visuospatial skills and language. There are various potential causes of dementia, but the most common include a range of neurodegenerative diseases, such as Alzheimer’s disease (AD) and dementia with Lewy bodies (DLB). We now know that some of these brain diseases may have been progressing for many years before the clinical symptoms are apparent, which unfortunately means that by the time dementia is clinically diagnosed, significant changes in the brain have already occurred, limiting the treatment options which can have any meaningful impact.
Doctors can provide a diagnosis of the brain diseases which lead to dementia based on certain tests and observable features, but it’s important to remember that despite decades of research we still do not have reliable biological markers for these diseases to provide accurate diagnosis, which typically can only be confirmed after death when the brain can be examined; known as a post-mortem neuropathological assessment. The accuracy of clinical diagnosis in life has been reported to be between 70 and 80%, which shows that determining which brain disease is causing dementia in an individual can be a challenge and may be complicated by the presence of multiple disease pathologies.
Post-mortem neuropathological assessment is not routine, but it is important for accurate disease diagnosis and for advancing our understanding of how these brain diseases develop and progress. But what does a neuropathological assessment actually involve? Hospitals, research institutes, and brain banks may vary in terms of their local processes and procedures, but once the brain is retrieved it will typically be placed in a solution called formalin for two weeks to preserve and fixate the brain, so the tissue is suitable for dissection. The assessing neuropathologist will begin the examination by looking for any significant macroscopic changes to the brain, such as whether the two hemispheres of the brain are symmetrical, and whether there are any contusions. Weighing the brain can also give a quick indication of whether there is any general atrophy, or loss of brain tissue. During dissection, key changes to look out for which would be indicative of neurodegenerative disease include enlarged ventricles, cerebral atrophy, and tissue discolouration. For example, typical changes associated with AD would include cerebral atrophy across all four lobes of the brain, but most extensively in the medial temporal lobe.
For the brain to be assessed microscopically, it is dissected into smaller parts focussing on specific regions of interest which require more detailed examination. These samples are embedded in blocks of paraffin wax which preserves the tissue and allows for very thin sections to be cut for histological staining. Consensus criteria has been produced for neuropathological diagnosis of neurodegenerative diseases, so immunohistochemistry methods can be used to detect and visualise in cut brain sections the pattern and distribution of certain proteins which are determined to be characteristic features of particular brain diseases.
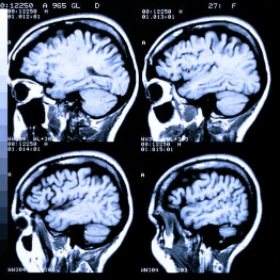
MRI scans are very good for looking at the brain, and very helpful to a neuropathologist when scans taken during life are combinted with examination of postmortem tissue.
In AD, for example, microscopic examination shows deposits of amyloid which clump together into plaques that collect between neurons disrupting cell function. The type of plaques which are present is important because non-fibrillary diffuse plaques are actually commonly associated with typical ageing, and it is the neuritic plaques with thickened neuronal processes which are associated with disease. In addition to amyloid plaques, we also see clumping together of a protein called tau into tangles inside neurons which affects cell communication. Both amyloid and tau are commonly found in the hippocampus which is one of the brain regions involved in the processing of memories, so it is no surprise that memory impairment is significant in AD. As the disease progresses, other brain regions see plaques and tangles accumulate. However, the presence of these neuropathologies does not simply lead to a clear diagnosis of AD. Other neurodegenerative diseases, like DLB, will typically see a comparable pathological profile to AD on the microscopic level, but with the addition of Lewy bodies which consist of the synaptic protein α-synuclein. Similarly, chronic traumatic encephalopathy is a neurodegenerative disease associated with a history of traumatic brain injury, and again shows a comparable pathological profile to AD on the microscopic level. However, the accumulated tau is particularly distributed at the depths of cortical sulci in a patchy pattern, which is a distinguishing feature for diagnosis. Neuropathological assessment at the microscopic level therefore needs to cover a range of possible neuropathologies, taking into account their pattern and distribution in order to determine the primary cause of the dementia.
It is worth noting that multiple disease pathologies are common in people who have had dementia, making neuropathological diagnosis all the more challenging. But it is important if we want to understand what causes these brain diseases to develop in order to create treatments which halt progression of developing pathologies, or ideally prevent them altogether. These treatments will have little benefit unless delivered early in the disease process, which brings us back to the need for accurate diagnosis of neurodegenerative disease in life. It is possible that advances in brain scanning and assessment of fluid biomarkers could provide the breakthrough we need for early disease detection, but at least for the most common neurodegenerative diseases they would need to distinguish the pattern and distribution of progressing neuropathologies which are characteristic of these brain diseases.

Dr Kamar Ameen-Al
Author
Dr Kamar Ameen-Ali is a Research Associate at University of Glasgow, exploring how neuroinflammation following traumatic brain injury contributes to the progression of neurodegenerative diseases that lead to dementia. Having first pursued a career as an NHS Psychologist, Kamar went back to University in Durham to look at rodent behavioural tasks to completed her PhD, and then worked as a regional Programme Manager for NC3Rs. Kamar brings a wealth of experience and writes on a range of topics from her time in the NHS, working for a Research Funder and from her work and life in the lab.

 Print This Post
Print This Post




